6 Facts About Deep Vein Thrombosis
Deep vein thrombosis occurs when the blood flow in a vein deep inside the body is blocked or slowed. It is often undiagnosed, but it is a serious medical condition. Deep vein thrombosis is the third leading vascular diagnosis in the U.S. each year after heart attacks and strokes.
Anyone can develop the condition, and it is treatable when caught early. Here are six facts you need to know about deep vein thrombosis.
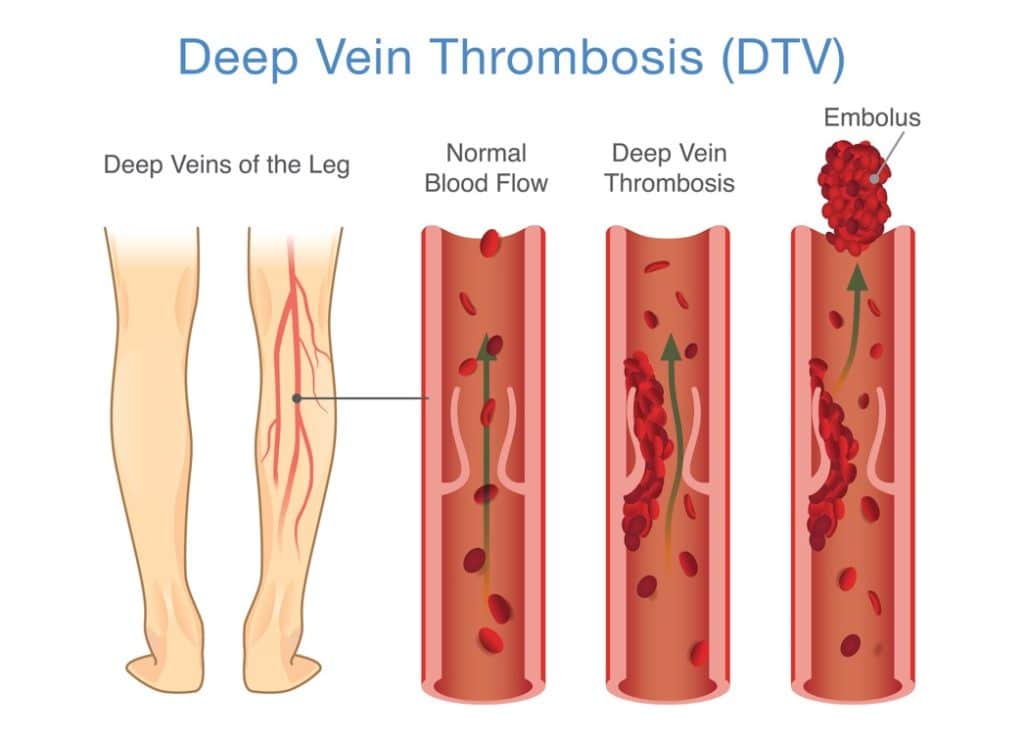
1. Deep vein thrombosis usually occurs in the legs
The lower part of your body is more susceptible when blood flow slows or pools in the veins, causing a blockage that turns into a clot called venous thromboembolism. It occurs in the blood vessels in the legs more often but can happen in the pelvis or arms.
2. Symptoms may not be apparent
The symptoms can include leg pain and swelling, cramping or soreness in the calf. The area may feel warm to the touch, and your skin color may look red or purplish. However, half of the people diagnosed with deep vein thrombosis may not have symptoms at all.
3. Risk factors can vary
The condition can develop for several reasons. It commonly develops in people over 50 but can happen at any age. These risk factors contribute to the likeliness of having deep vein thrombosis, and the more you have, the more at risk you are of developing the condition.
- Prolonged inactivity or being on bed rest, which reduces blood flow
- Injury to bones that have damaged the veins
- Varicose veins that become swollen and twisted
- Excess body weight, which more pressure on the veins in your legs
- Certain cancers that increase the risk of blood clots
- Heart failure or other conditions makes the heart work harder to pump blood
- A history of the condition in your family
- If you have had a blood clot before
- Smoking, which affects how blood flows
- Pregnancy, which causes increased estrogen, a hormone that causes blood to clot more easily
4. Treatments are available
Deep vein thrombosis treatment is available. The goal of treating the condition is to keep clots from getting bigger, prevent them from breaking off and reduce your chance of developing another one. After a full exam to determine the potential causes of the condition, your doctor will create a treatment plan that may include one of the following:
Medication
Anticoagulants, or blood thinners, are often used to treat the condition because they prevent clotting and make it harder for venous thromboembolism to occur. They can cause a risk of increased bleeding. A doctor should monitor your blood thinner usage when used for treatment.
Compression socks
Symptoms can be relieved by compression socks or stockings, which produce constant pressure to promote blood flow in the legs. They are usually tightest at your ankle and looser around your upper legs to ensure blood is getting to your heart. Your doctor can recommend the level of compression you need.
Surgery
Your doctor may recommend a thrombectomy if you have large clots or cannot use blood thinners because of another condition. During the surgery, the doctor will remove the clot by making an incision in the vein, then repair it and the surrounding tissue.
5. You can prevent deep vein thrombosis
Prevention is key when it comes to this condition. If you have any of the risk factors listed above, consider changing your lifestyle to reduce your chances of developing a blood clot.
Exercise in any form will get the blood flowing in your lower body and strengthen the muscles that help pump blood to your heart. If you sit for long periods, walk around a few times each day to stretch your legs and increase circulation. Moderate daily exercise can help you lose the weight contributing to the condition.
If you are at risk for deep vein thrombosis because of another condition, talk to your doctor to learn strategies for reducing your chance of developing it.
6. This condition can be dangerous
Deep vein thrombosis can cause life-threatening complications. When blood flow is blocked, a clot called venous thromboembolism can form. The clot can break off and travel to the lungs, causing a blockage called pulmonary embolism, which can be fatal.
Symptoms of pulmonary embolism include:
- Shortness of breath that comes on suddenly
- Chest pain or discomfort
- Feeling dizzy, lightheaded or fainting
- Rapid pulse
- Coughing up blood
If you are experiencing any of the symptoms above in relation to suspected deep vein thrombosis, seek medical help immediately.
When to see a deep vein thrombosis doctor
If you are concerned that your health or medical conditions may be causing deep vein thrombosis, schedule an appointment with a doctor. Your primary care physician may recommend that you see a hematologist who specializes in diagnosing and treating blood conditions. Personalized Hematology-Oncology & Primary Care has skilled physicians who can diagnose and treat your condition. Contact us today to make an appointment.